Bacterial Agents
Previously links from this site included links to US government and other agency websites, due to the actions of Donald Trump, some of these may no longer be regarded as reliable, and some have been closed down, therefore I have linked to other sites.
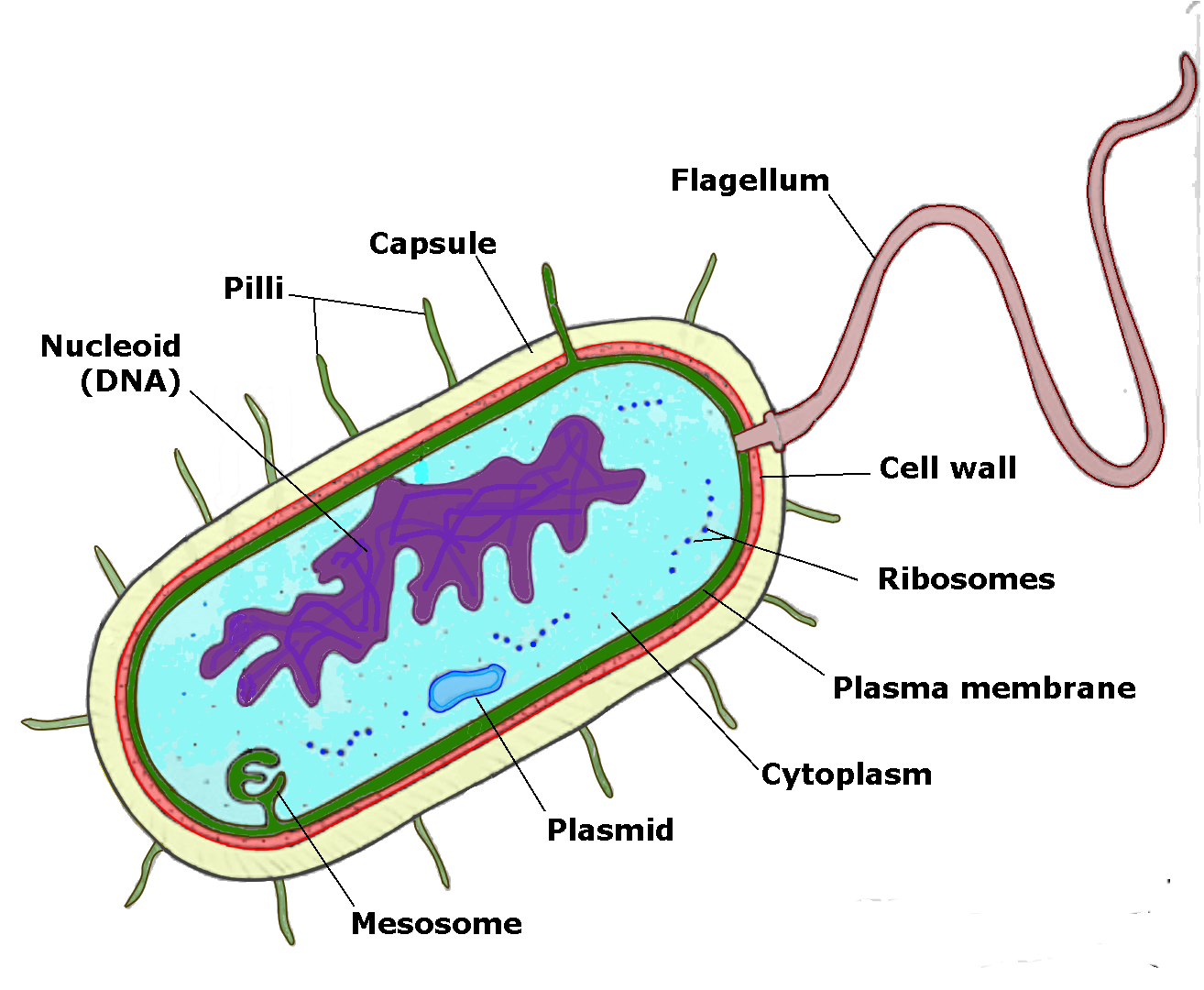
Bacterial cell structure
Bacteria are single celled organisms which typically range in size 0.3µm to 14µm (1µm = 1/1000 of a millimetre). Whilst exceedingly small they are fully functioning organisms, obtaining their nutrition from their environment, and able to manufacture the complex substances necessary for life and reproduction. The cell structure is simpler than that of other organisms as there is no nucleus nor are there membrane bound organelles. Instead their control centre containing the genetic information is contained in a single loop of DNA. Some bacteria have an extra circle of genetic material called a plasmid. The plasmid often contains genes that give the bacterium some advantage over other bacteria. For example it may contain a gene that makes the bacterium resistant to a certain antibiotic.
Bacteria vary enormously in the substances which they can utilise as food and the environments they can survive in, from high altitude to the bottom of the deepest seas, to hot sulfur springs and even storage pools for nuclear waste. Whilst some organisms can survive in a wide range of situations, others are extremely specific.
Microbiologists classify bacteria by a variety of means including: shape, motility, reactions to various stains, whether or not they need oxygen to survive, their ability to utilise different energy sources, their appearance when grown in the laboratory, whether or not they ferment certain sugars and the temperatures at which they live. The cell diagram at the top of the page shows the major features of a bacterial cell, however not all bacteria show all features.
Bacterial morphology
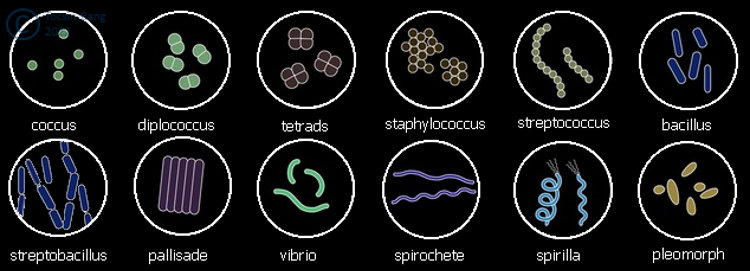
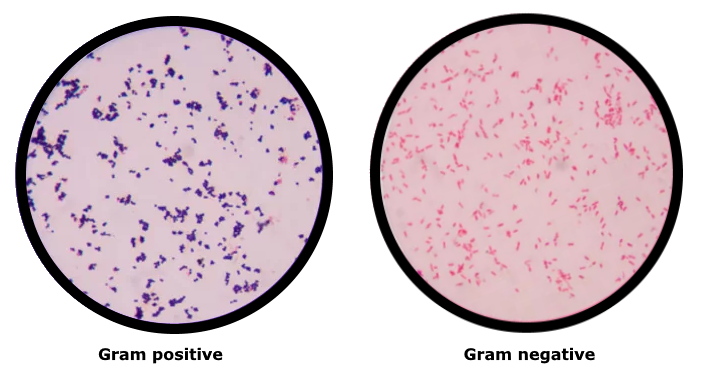
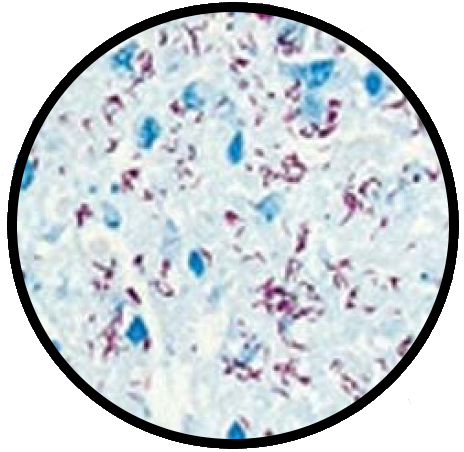
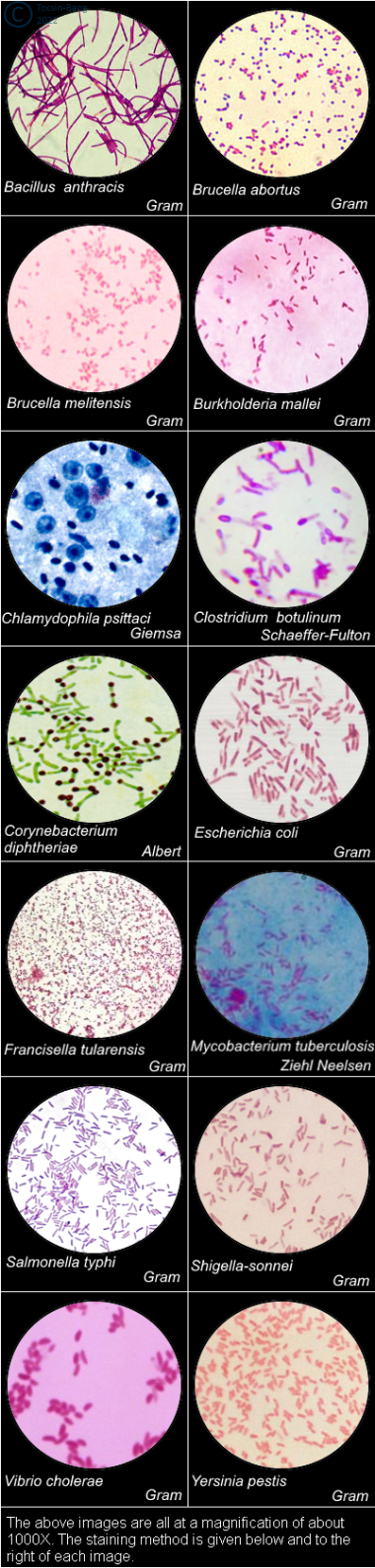
Bacteria are, in part, classified into groups according to their basic shapes or morphology: spherical (cocci), rod (bacilli), spiral (spirilla), comma (vibrios) or corkscrew (spirochaetes). They can exist as single cells, in pairs, chains or clusters.Staining methods are also used in identifying bacteria. The best known staining methods for bacteria are Gram's stain and Ziehl-Neelsen acid-fast staining. Other common methods include Albert's, Giemsa, negative and silver stains
Gram's stain
Hans Christian Gram developed what is perhaps the most famous of bacteriological stain in 1884. Gram's stain divides all bacteria into one of two groups, gram positive and gram negative. There are numerous variations of the Gram staining method, in fact it was the subject of the first research project I conducted back in 1966. Fundamentally a film of bacteria is spread on a microscope slide and then heat fixed by passing through a flame three or four times. The method may also be used on histological sections, with some minor variations of technique. The film, is then flooded with a solution of crystal violet for a few seconds. Next the slide is washed and then flooded with dilute iodine solution. Following this an attempt is made to remove the stain using 70% ethanol (some methods use acetone or an acetone/ethanol mixture), this only lasts about 10 seconds. The smear is then counter-stained with a red or yellow stain. Bacteria that retain the crystal violet/iodine complex and appear blue/black are said to be Gram positive.
Ziehl-Neelsen stain
This method was developed by Franz Ziehl and Friedrich Neelsen in the mid 1890s. In acid fast staining bacteria are differentiated according to whether or not, after staining, they can be decolourised by dilute sulfuric or hydrochloric acid, the best known of these staining methods is Ziehl-Neelsen. A heat killed smear or histological section is first stained with carbol-fuchsin (solution of the red dye fuchsin in a solution of phenol. The slide is then washed in water, and an attempt to remove the stain is made using either dilute hydrochloric or sulfuric acid or acidified alcohol. The preparation is then counter-stained with either a blue or green stain, typically methylene blue. Acid-fast organisms show up as red.
Potential Bacterial agents
The letters in (brackets) represent the NATO military codename(s). The letters in [square brackets] represent the National Center for Emerging and Zoonotic Infectious Diseases (NCEZID) classification of organisms.Bacillus anthracis - (N or TR), [Cat A]
Bacillus anthracis causes anthrax and is one of the most deadly agents to have been used as a biological weapon. It is classified by the US Centers for Disease Control and Prevention (CDC) as a Category A agent, posing a significant risk to national security. The gram-positive, rod-shaped anthrax spores are found naturally in soil, can be easily cultured in a laboratory, and last for many years, as spores, in the environment. Anthrax has been used as a biological weapon for about a century. Letters containing powdered anthrax spores were intentionally mailed through the US postal system in 2001 affecting 22 people of which five died. Experiments with the use of anthrax have been undertaken by all countries attempting to use biological weapons.Brucella abortus - [Cat B]
Brucella abortus causes contagious abortion in ruminants and brucellosis in humans. Brucella abortus is a Gram-negative rod shaped bacteria that is non-motile, nor does it create capsule slime. It does produce endospores, which enable survival under long-term starvation and dessication. This heterotrophic bacterium carries out either aerobic or anaerobic respiration. This bacterium, as an intracellular pathogen, enters phagocytes, such as macrophages, in humans and in cows. It attaches to the endoplasmic reticulum of these cells. In humans brucellosis has both an acute and a chronic phase. The chronic phase will last as long as the host is alive without treatment. Acute symptoms include fever, chills, headache, backache, weakness, and weight loss. The chronic symptoms are usually recurring joint pain, fatigue, and headaches. There is an antibiotic regimen for humans who come in contact with the disease that includes the antibiotics rifampin and doxycycline together.
Brucella melitensis - (AM or BX) [Cat B]
Brucella melitensis is a Gram-negative coccobacillus bacterium from the Brucellaceae family. The bacterium causes ovine and caprine brucellosis. It affects primarily sheep and goats, but cases have also been observed in cattle, yaks, water buffalo, camels, alpacas, dogs, horses and pigs. Humans can become infected. B. melitensis is the most pathogenic of the brucellae, for humans.
Brucella suis - (US, AB or NX) [Cat B]
Brucella suis, the cause of porcine brucellosis, can also infect humans. Brucella suis is a Gram-negative, facultative, intracellular coccobacillus, capable of growing and reproducing inside of host cells, specifically phagocytic cells. They are not spore-forming, capsulated, or motile. B. suis was the first biological agent weaponized in 1952 in the USA, and was field-tested with B. suis-filled bombs called M33 cluster bombs. It is, however, considered to be one of the agents of lesser threat because many infections are asymptomatic and the mortality is low, but it is used more as an incapacitating agent.
Burkholderia mallei - [Cat B]
Burkholderia mallei is the cause of glanders, a zoonotic disease that primarily affects horses, donkeys, and mules, but can also be seen in other animals e.g. goats, dogs, and cats. Glanders is rare in humans. B. mallei is a Gram-negative, coccobacillius it is non-motile and aerobic. During World War I, the Germans used B. mallei to infect animals that were being sent from neutral countries to the Allies with glanders.
Burkholderia pseudomallei - (HI) [Cat B]
Burkholderia pseudomallei the cause of melioidosis in humans also known as Whitmore's disease. B. pseudomallei is practically identical to B. mallei (they share about 99% of their DNA), to the extent that it is very difficult to tell them apart, and some authorities regard them as different strains of the same organism. B. pseudomallei is a Gram-negative, coccobacillius, it is non-motile and aerobic. There are several types of melioidosis infection, each with their own set of symptoms. It is important to note that melioidosis has a wide range of signs and symptoms that can be mistaken for other diseases such as tuberculosis or more common forms of pneumonia.
Chlamydophila psittaci - (SI) [Cat B]
Chlamydophila psittaci is a lethal intracellular bacterial species that may cause endemic avian chlamydiosis, epizootic outbreaks in mammals, and respiratory psittacosis in humans. C. psittaci undergoes several transformations during its lifecycle it exists as an elementary body (EB) between hosts The EB is not biologically active, but is resistant to environmental stresses and can survive outside a host. The lifecycle of C. psittaci is divided between the elementary body which is able to infect new hosts, but cannot replicate, and the reticulate body, which replicates, but is not able to cause new infection.
Clostridium botulinum - [Cat A]
Clostridium botulinum is a Gram-positive, rod-shaped, spore-forming bacterium, its toxins cause botulism. It is an obligate anaerobe, meaning that oxygen is poisonous to the cells. However, C. botulinum tolerates traces of oxygen due to the enzyme superoxide dismutase, which is an important antioxidant defense in nearly all cells exposed to oxygen. C. botulinum forms protective spores when conditions for survival are poor. The spore has a hard protective coating that encases the key parts of the bacterium and has layers of protective membranes. Within these membranes and the hard coating, the dormant bacterium is able to survive for years. C. botulinum produces seven neurotoxins (types A-G). These are the most potent toxins known (as little as 30 ng is sufficient to cause illness and possibly death), and are responsible for botulism, a severe and often fatal neuroparalytic intoxication. Two related organisms Clostridium butyricum and Clostridium baratii may also produce the same toxins.
Corynebacterium diphtheriae - (DK)
Corynebacterium diphtheriae the cause of diphtheria, is a nonmotile, aerobic, noncapsulated, club-shaped, Gram-positive rod-shaped bacterium. Some strains produce a potent exotoxin. C. diphtheriae is only able to produce its exotoxin when the bacterium is infected by a bacteriophage which provides it with the toxin-producing gene. The symptoms of diphtheria include pharyngitis, fever, swelling of the neck or area surrounding the skin lesion. Diphtheritic lesions are covered by a pseudomembrane. The toxin is distributed to distant organs by the circulatory system and may cause paralysis and congestive heart failure.
Coxiella burnetii - [Cat B]
Coxiella burnetii is an obligate intracellular bacterial pathogen, and is the causative agent of Q fever. C. burnetii is a small Gram-negative, cocco-bacillary bacterium that is highly resistant to environmental stresses such as high temperature, osmotic pressure, most disinfectants and ultraviolet light. C. burnetii was originally classified as a rickettsia, but when differences from other rickettsia became apparent it was assigned its own genus. C. burnetii is one of the most infectious organisms known, only 1-10 organisms are needed to infect 50% of the population. C. burnetii is one of seven biological organisms that were weaponised by the USA during their biological warfare programme.
Escherichia coli - (Y) [Cat B]
Escherichia coli is a Gram-negative, facultative anaerobic, rod-shaped, coliform bacterium of the genus Escherichia that is commonly found in the lower intestine of warm-blooded organisms. Most E. coli strains are harmless, but virulent strains can cause gastroenteritis, urinary tract infections, neonatal meningitis, hemorrhagic colitis, and and has been implicated in Crohn's disease. The harmless strains are part of the normal microbiota of the gut, and can benefit their hosts by producing vitamin K2, and preventing colonisation of the intestine with pathogenic bacteria. Under favorable conditions, it takes as little as 20 minutes to reproduce.
Francisella tularensis - (SR or JT) [Cat A]
Francisella tularensis is the cause of tularaemia, also known as Pahvant Valley plague, rabbit fever, deer fly fever, and Ohara's fever. Tularaemia is a bacterial zoonotic disease of the northern hemisphere. F. tularensis is an aerobic Gram-negative coccobacillus. It is a non-sporing and non-motile organism. In nature, the disease may be spread in a number of ways, person to person by droplet infection, by arthropod vector, or contact with infected animals, or ingestion of contaminated water or food. The Soviet Red Army used F. tularensis against German troops in the battle of Stalingrad during World War II.
Listeria monocytogenes
Listeria monocytogenes is a facultative anaerobic, Gram positive, rod-shaped, motile, non-spore forming bacterium. It can grow and reproduce inside the host's cells and is one of the most virulent food-borne pathogens: 20 to 30% of foodborne listeriosis infections in high-risk individuals may be fatal. L. monocytogenes is able to reproduce at 0°C. Invasive infection by L. monocytogenes causes the disease listeriosis. When the infection is not invasive, any illness as a consequence of infection is termed febrile gastroenteritis. The manifestations of listeriosis include sepsis, meningitis (or meningoencephalitis), encephalitis, corneal ulcer, pneumonia, and intrauterine or cervical infections in pregnant women, which may result in spontaneous abortion in the second to third trimester or stillbirth.
Mycobacterium tuberculosis - [Cat C]
Mycobacterium tuberculosis the cause of tuberculosis has an unusual, waxy coating on its cell surface primarily due to the presence of mycolic acid. This coating makes the cells impervious to Gram staining, and as a result, M. tuberculosis can appear either Gram-negative or Gram-positive. Acid-fast stains such as Ziehl-Neelsen, or fluorescent stains such as auramine are used instead to identify M. tuberculosis microscopically. M. tuberculosis is rod-shaped, a strict aerobe, is non-sporing, and is non-motile. M. tuberculosis is unusually slow growing, reproducing by binary fission every 18-24 hours. Primarily a pathogen of the mammalian respiratory system, it normally infects the lungs. M. tuberculosis is a member of a group of closely related organisms comprising: M. tuberculosis, M. paratuberculosis (the cause of Johne's disease in ruminants, M. africanum, M. orygis. M. bovis (the primary cause of bovine tuberculosis) and the Bacillus Calmette-Guérin strain (used in vaccination against tuberculosis), M. microti, M. canetti, M. caprae, M. pinnipedii, M. suricattae, and M. mungi. M. tuberculosis is an unlikely BW agent because of its slow growth, and the fact that the majority of the population have been immunised.
Rickettsia prowazekii - (YE)
Rickettsia prowazekii is a small, Gram-negative, obligately intracellular, rod-shaped bacterium. R. prowazekii is the causative agent of epidemic typhus, also called louse-borne typhus. Epidemic typhus is spread to people through contact with infected body lice. Symptoms of epidemic typhus begin within 2 weeks after contact with infected body lice. Signs and symptoms may include: fever and chills, headache, rapid breathing, body and muscle aches, rash, cough, nausea, vomiting, and confusion. Some people can remain infected, without symptoms, for years after they first get sick.
Rickettsia rickettsii - (RI or UY)
Rickettsia rickettsii the cause of Rocky Mountain spotted fever (RMSF), is a Gram-negative, intracellular, coccobacillus bacterium that is around 0.8 to 2.0 μm long. R. rickettsii is one of the most pathogenic of Rickettsia. The most common cause of infection is bites by infected ticks. The most common hosts for R. rickettsii are ticks in the family Ixodidae. Typical symptoms of RMSF can appear 2 - 14 days after exposure and include fever, headache, depression, nausea, vomiting, and a skin rash called purpura or petechiae. Sometimes the rash occurs 2 to 5 days after the onset of the fever. Serious cases of RMSF can include central nervous system, pulmonary, or hepatic injuries.
Rickettsia typhi - (AV)
Rickettsia typhi is a small, Gram-negative, rod-shaped, obligately intracellular bacterium. R. typhi is the cause of murine or endemic typhus. R. typhi is transmitted primarily by the rat flea, Xenopsylla cheopis, although lice and mites are also potential vectors. Rodents (mainly Rattus norvegicus, and Rattus rattus) are considered the main reservoir of bacteria, but other vertebrate hosts may serve as reservoir including house mice, shrews, opossums, skunks, and cats. Murine typhus symptoms are similar to those of epidemic typhus, although the former is usually less severe. The incubation period is usually more prolonged than that of epidemic typhus. Symptoms include headache, arthralgia and ill feeling, with or without a low grade fever. Onset is characterized by persistent headache, a high grade fever, and a cutaneous rash predominating on the trunk. The rash is usually less apparent than in epidemic typhus, and occasionally absent.
Salmonella enterica
Salmonella enterica - are rod-shaped, motile, facultative aerobic, Gram-negative bacteria. S. enterica contains a large number of serovars or serotypes, which can infect a broad range of vertebrate hosts. The individual members range from being highly host-adapted to those displaying a broad host range The most significant serovars as far as human disease is concerned are: Enteritidis, Hadar, Heidelberg, Infantis, Paratyphi, Typhi, and Typhimurium. In fact there are more than 2,500 serovars. Of these the last three are considered to be potential BW agents.
- S. enterica Paratyphi, there are three varieties of S. enterica Paratyphi, A, B, & C. They cause paratyphoid, a potentially severe and occasionally life-threatening bacteraemic illness. While fever and gastrointestinal symptoms are common, the clinical presentation varies, including mild and atypical infections. Infections caused by Salmonella enterica serotypes Paratyphi A, B (tartrate negative), and C are often characterized by insidious onset of sustained fever, headache, malaise, anorexia, relative bradycardia, constipation or diarrhea, and non-productive cough. However, mild and atypical infections may occur.
- S. enterica Typhi, is the cause of typhoid fever a systemic infection, usually through ingestion of contaminated food or water. The acute illness is characterized by prolonged fever, headache, nausea, loss of appetite, and constipation or sometimes diarrhoea. Symptoms are often non-specific and clinically non-distinguishable from other febrile illnesses. However, clinical severity varies and severe cases may lead to serious complications or even death.
- S. enterica Typhimurium, is the cause of paratyphoid fever a life-threatening illness. The acute illness is characterised by a sustained fever that can be as high as 39 - 40°C, weakness, abdominal pain, headache, diarrhea or constipation, cough, loss of appetite. Some people with paratyphoid fever develop a rash of flat, rose-colored spots.
Shigella spp. - [Cat B]
Shigella spp. cause the infectious, intestinal human disease shigellosis, they are non-spore forming, non-motile, rod-shaped Gram-negative bacteria. Most who are infected with Shigella develop diarrhea, fever, and stomach cramps starting a day or two after they are exposed to the bacteria. Shigellosis usually resolves in 5 to 7 days. Some people who are infected may have no symptoms at all, but may still pass the Shigella bacteria to others. Members of the genus are highly infectious, and cause 1 million deaths annually worldwide.
- S. dysenteriae serogroup A causes deadly epidemics mainly in developing countries,
- S. boydii serogroup C
is restricted to the Indian subcontinent,
- S. flexneri serogroup B and is responsible for the worldwide endemic form of shigellosis
- S. sonnei serogroup D are prevalent in developing and developed countries, respectively.
Vibrio cholerae - [Cat B]
Vibrio cholerae - the cause of cholera, is a Gram-negative, comma-shaped, halophilic, a facultatively anaerobic, highly motile bacterium. Cholera is a diarrheal disease, easily mistakable for several others; however, there are some clinical features that are characteristic and can help make the diagnosis. The presence of watery diarrhea with the appearance of rice wter is characteristic. This is even more impressive when associated with acute severe dehydration. Other symptoms may include: abdominal pain, vomiting, cramping rectal pain and other cramps, abnormally slight or infrequent urination, dry mucosae, fever is less common, mental status alteration, from alert to restless, somnolent and even comatose
Yersinia pestis - (LE), [Cat A]
Yersinia pestis the cause of plague is a gram-negative, non-motile, non-sporing, rod-shaped, facultatively anaerobic, coccobacillus bacterium. Symptoms of plague include fever, weakness and headache. Usually this begins one to seven days after exposure. There are three forms of the disease. In the bubonic form there is also swelling of lymph nodes, while in the septicemic form tissues may turn black and die, and in the pneumonic form shortness of breath, cough and chest pain may occur. Bubonic and septicemic plague are generally spread by flea bites or handling an infected animal. The pneumonic form is generally spread person to person through the air via infectious droplets.
- Bubonic plague - When an infected flea bites a human and contaminates the wound with regurgitated blood, the plague-causing bacteria are passed into the tissue. Y. pestis can reproduce inside cells, so even if phagocytosed, they can still survive. Once in the body, the bacteria can enter the lymphatic system. Y. pestis spreads through the lymphatic vessels of the infected person until it reaches a lymph node, where it causes acute lymphadenitis. The swollen lymph nodes form the characteristic buboes associated with the disease. If the lymph node is overwhelmed, the infection can pass into the bloodstream, causing secondary septicemic plague and if the lungs are seeded, it can cause secondary pneumonic plague.
- Septicemic plague - The lymphatic system ultimately drains into the bloodstream, so the plague bacteria may enter the blood and travel to almost any part of the body. In septicemic plague, bacterial endotoxins cause disseminated intravascular coagulation (DIC), causing tiny clots throughout the body and possibly ischemic necrosis (tissue death due to lack of circulation) from the clots. DIC results in depletion of the body's clotting resources, so that it can no longer control bleeding. Consequently, there is bleeding into the skin and other organs, which can cause red and/or black patchy rash and haemoptysis an haematemesis. There are bumps on the skin that look somewhat like insect bites; these are usually red, and sometimes white in the center. Untreated, septicemic plague is usually fatal. People who die from this form of plague often die on the same day symptoms first appear.
- Pneumonic plague - The pneumonic form of plague arises from infection of the lungs. It causes coughing and thereby produces airborne droplets that contain bacterial cells and are likely to infect anyone inhaling them. The incubation period for pneumonic plague is short, usually two to four days, but sometimes just a few hours. The initial signs are indistinguishable from several other respiratory illnesses; they include headache, weakness and spitting or vomiting of blood. The course of the disease is rapid; unless diagnosed and treated soon enough, typically within a few hours, death may follow in one to six days; in untreated cases mortality is nearly 100%.